-
Can MASTOCHECK be used as a standalone diagnostic test?
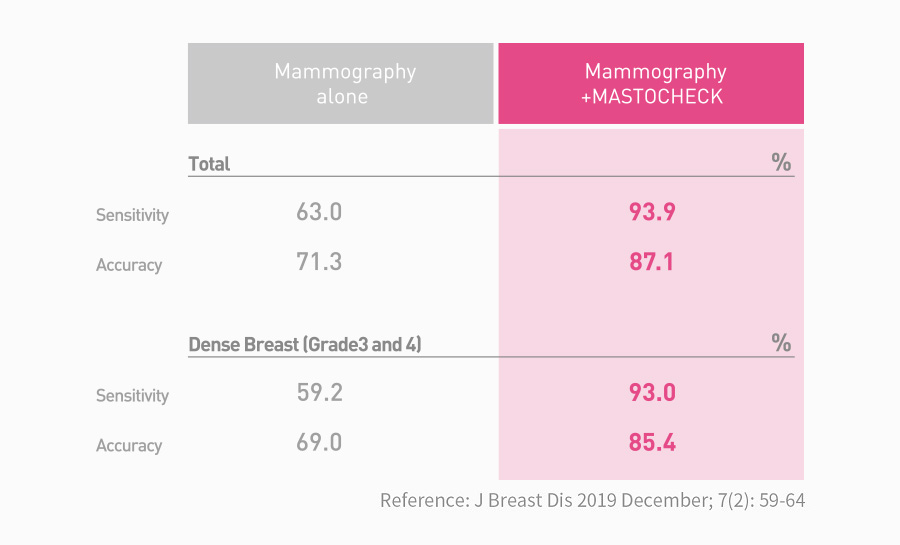
While MASTOCHECK demonstrates high diagnostic accuracy on its own, it’s effectiveness can be increased when used in combination with mammography. When combined, the overall sensitivity increases to 93.9%, and it maintains a high sensitivity of 93% even in women with dense breast tissue (grades 3 and 4).
-
Is fasting required before the test?
No, fasting is not required for MASTOCHECK.
-
How does it differ from the genetic test?
Genetic tests, such as BRCA1 or BRCA2, are used to assess inherited risk and determine whether someone has a higher likelihood of developing breast cancer. They do not detect whether cancer is currently present.�In contrast, MASTOCHECK is a blood-based test that analyzes specific protein biomarkers to help identify the actual presence of breast cancer at the time of testing.
-
Is MASTOCHECK a reliable test?
MASTOCHECK is the result of years of clinical research led by Professor Dong-Young Noh, a key opinion leader in breast oncology, and his team at Seoul National University in Korea. It has demonstrated clinical effectiveness in detecting early-stage breast cancer (phases 0–2) and has been approved as an in vitro diagnostic medical device by the Korean Ministry of Food and Drug Safety.
-
Besides breast cancer do other cancer types affect the test result?
Biomarkers for MASTOCHECK have almost no correlation with lung, stomach, liver, ovarian, uterus, colon, pancreatic cancer, and more.
The test specializes in diagnosing breast cancer by using breast cancer-specific biomarkers.
-
What is the recommended MASTOCHECK screening cycle?
We recommend patients to undergo MASTOCHECK screening annually, unless they are considered high risk due to personal or familial factors.
The one-year interval is recommended because proteins in the blood vary with lifestyle habits as well as with environmental factors.
-
Does a ‘high-risk’ result mean I have breast cancer?
MASTOCHECK is a breast cancer screening tool, not a definitive diagnostic test like a biopsy. A ‘high-risk’ result does not confirm the presence of cancer, but it does indicate the need for further evaluation. We recommend consulting a medical professional and undergoing additional diagnostic tests for confirmation.